This page will provide an overview of the Quality Performance Category of MIPS.
The influence of the quality score on the final MIPS performance score
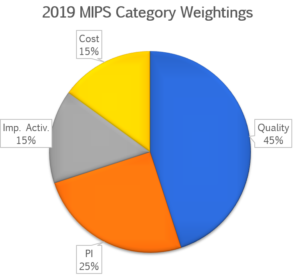
The MIPS quality performance category is weighted at 45% of the MIPS score in the 2019 performance year for most clinicians, groups and virtual groups. This may change for certain clinician types and when practices meet exclusions, re-weightings, or exceptions for performance in other categories.
The following are examples of where the quality category weighting may be increased:
- If the practice does not have an adequate number of cost measure episodes attributed to a clinician and/or TIN. The 15 cost points are then redistributed to the quality category.
- The following clinician types, all newly eligible for the MIPS in 2019, are not scored on the promoting interoperability or the cost category. They receive a weighting of 70% quality and 30% improvement activities. Note that this is not accurate if the practice is a group that includes physicians.
- Physical therapists
- Occupation therapists
- Qualified speech-language pathologists
- Qualified audiologists
- Clinical psychologists
- Registered dieticians/nutrition professionals
- The following clinicians and clinician types are not required to submit promoting interoperability data (this category is automatically reweighted to 0%) and the 25 points from this performance category are reallocated to the quality performance category. This is only true if they are not members of a group that includes physicians.
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Certified nurse anesthetists
- MIPS eligible clinicians that work in ambulatory surgery centers
- Non-patient-facing clinicians in groups
- All clinicians and groups that qualify for a hardship exemption for the promoting interoperability category
How is scoring determined in this category?
The maximum score in this category is 60 points or 70 points depending on practice size. Small practices, those of 15 or fewer clinicians, are scored on up to six quality measures, each worth a maximum of 10 points (not counting potential bonus points). Larger practices are also scored on up to six quality measures but they are also automatically scored on the All Cause Readmission Measure. Subspecialty practices may report fewer measures if there are less than six measures applicable to the practice type.
Clinicians select from over 340 quality measures. The scores on each measure are essentially a numerator/denominator ratio. The eligible population for the measure is included in the denominator and when the performance requirement is met for an encounter in the denominator population, is populated in a numerator.
For example if the practice saw 100 patients during the year that had a history of current tobacco abuse, and they provided cessation counseling to 99 of the 100 patients, they would have a “raw” MIPS score of 99% for the tobacco screening and cessation counseling measure. This performance score is then compared to a benchmark for most measures. Benchmarks generally are moderately to markedly elevated, making it difficult to achieve high scores for most measures without near-perfect performance.
The raw performance scores for each measure reported are then compared to a benchmark. The benchmarks may vary by submission type. Submission types include claims, registry, and EHR e-measure reporting. Large groups of 25 or more clinicians may also choose the CMS Web Interface submission type.
Certain measures do not have benchmarks for the 2019 performance year. If CMS does not collect an adequate amount of data during the performance year to determine a benchmark, the measure will receive a maximum score of three points.
The performance scores for each measure after being compared to a benchmark are then added to potential bonus points for each measure. Practices of any size can earn bonus points by submitting outcome measures (worth two bonus points) high-priority measures (worth one bonus point) and for reporting measures view the end-to-in electronic reporting method. Small practices automatically receive a six point bonus, added to their total quality performance score.
The computed scores for each measure, including all bonuses, are then summated to determine the total quality category performance score. This figure is then applied to the weighting of the quality category to determine the final MIPS score component from the quality category. For example, if a small practice achieved a score of 50 points of the maximum 60 points this category, they would have an 83% performance rate. If the weighting for the quality category was 45 points, the practice would earn 37.5 out of a possible 45 points in the quality category.
Reporting Period and Data Completeness Requirement
The quality performance category reporting period is the entire calendar year.
In addition, in 2019 practices must report performance on a minimum of 60% of all eligible encounters during the calendar year. This is referred to as the “data completeness requirement.” For small practices if the data completeness requirement is not met the practice will receive a maximum of three points, regardless of their actual performance score. For large practices that do not meet the data completeness requirement for measure, the maximum score is one point.
There is also a case minimum requirement. For most measures at least 20 cases must be reported in the denominator for the measure to receive its full score. For practices of all sizes if the case minimum is not met, the practice will receive three points for that measure.
The Anatomy of Quality Measures
Each quality measure has detailed specifications. The majority of the measures have been developed by specialty associations or clinical workgroups. The specification documents provide a significant amount of detail as to which types of encounters, procedures, and/or patients should be included in the denominator. In order for patients to be included in the denominator the encounter may require certain ICD-10-CM codes, certain CPT/HCPCS codes, or other clinical factors. The documents also often contain exceptions and exclusions as to which patients should not be included in denominator. An example of this is in the blood pressure screening measure where patients with a pre-existing diagnosis of hypertension are excluded from the measure.
The specification documents also include detailed guidance on how the performance can be met for the individual measure. When performance is met the encounter is included in the numerator for that measure.
A detailed understanding of the specific requirements for each quality measure is important, as actions taken to report quality performance must be associated with clinical documentation. Clinicians need to understand what is needed for documentation purposes to achieve performance met, to exclude patients from the measure’s population as warranted, and to understand what the coding requirements are for each measure.
Quality Performance Category Challenges
The specification documents are frequently difficult to interpret and their guidance may not directly apply in a number of clinical situations. Practices are encouraged to review the specification documents closely and to seek advice from experts as needed. MIPS audits started in 2019 and will focus in part on documentation supporting quality measure actions.
Practices that see patients at multiple sites are required to aggregate all data from all clinical sites were eligible patients for each chosen measure are seen. CMS requires that 60% of all eligible encounters be reported, regardless of practice site or electronic health record system used. Many vendors will perform data aggregation services, however, getting quality data is an export from certain systems, for example hospital systems, may require some effort.
The benchmarks are often challenging in that less-than-perfect scores may drop performance on a measure from 10 points to less than seven points, even if performance was not met for only one encounter. For this reason, in order to obtain high scores, practices will need a mechanism in place to capture patients there eligible for measure where performance is not been met. For some measures performance only needs to be met once during the entire performance period. This allows practices to meet the measures performance requirement on a subsequent visit.
For further information on strategies related to quality performance please contact us at info@apollohit.com
Disclaimer: the information in this article represents interpretations of information provided by CMS, interactions with CMS, and experience working with practices. Please review formal documentation provided by CMS for additional information.